This section introduces a relatively new area in dentistry, focusing on conditions like facial pain and trigeminal neuralgia that arise from interactions between bone and the immune system. In affected bone tissue, as we will detail later, increased levels of the inflammatory mediator CCL5 bind to opioid receptors on sensory nerve fibers, resulting in continuous pain signaling. This advanced understanding of the biochemical processes behind chronic pain allows us to provide more precise and effective treatments for patients with complex or persistent facial pain conditions.
This field has been evolving for some time, and as of 2022, 6,459 scientific articles have been published on the impact of the inflammatory mediator CCL5 on several systemic diseases. The most common among them include fibromyalgia, arthritis, ALS, and oncological diseases.
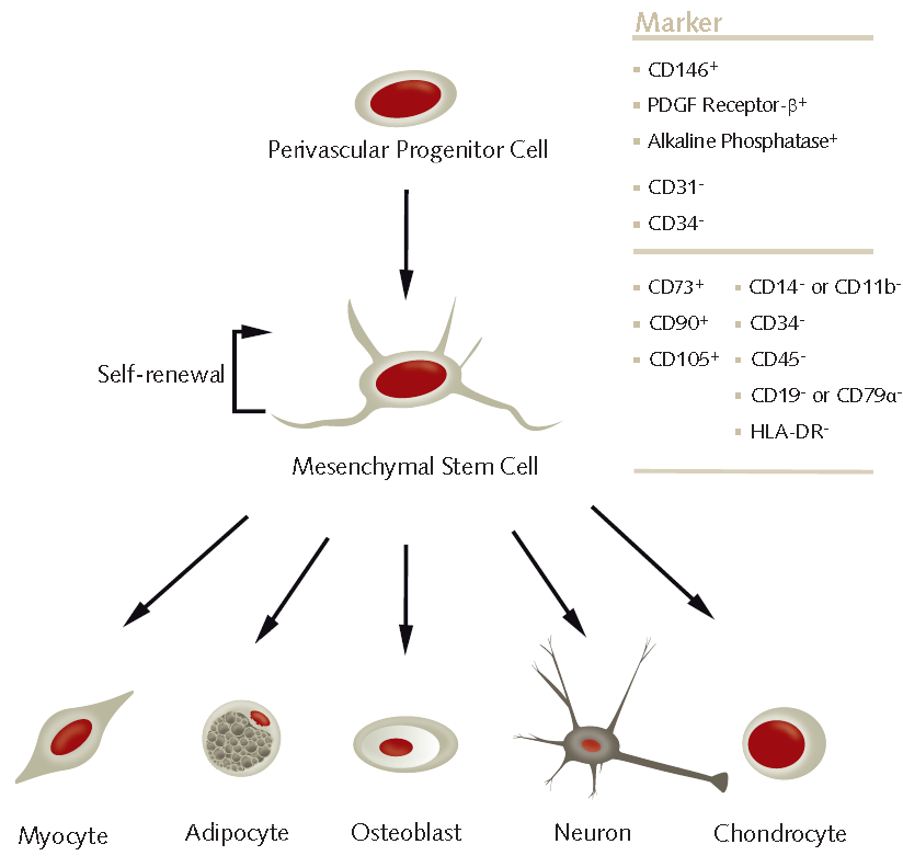
The diagram below illustrates the model of how a bone wound heals, for example, after tooth extraction. As we can see, the first month after the procedure is extremely important. A crucial step is the arrival of stem cells from your body into the wound. As we know, a stem cell can transform into various types of cells, thus beginning to perform their functions in the body.
In 1965, Professor Brånemark placed the first dental implant in the human body, and in 1985, he famously stated, “When I see a yellow bone, I cancel the implant surgery!” Why do we mention this here? Because FDOJ, by its tissue composition, is degenerative bone and fatty tissue. Clinically, it appears yellow, mixed with blood and bone fragments, and, as proven in our own studies, contains elevated levels of the inflammatory mediator CCL5. This mediator binds to CCR5 receptors found throughout the body. Constant release of the CCL5 chemokine means continuous activation of the CCR5 receptor, which is associated with chronic diseases and even cancer. For those interested, here are two relevant publications.(Nature, NCBI) izmed mnogih.
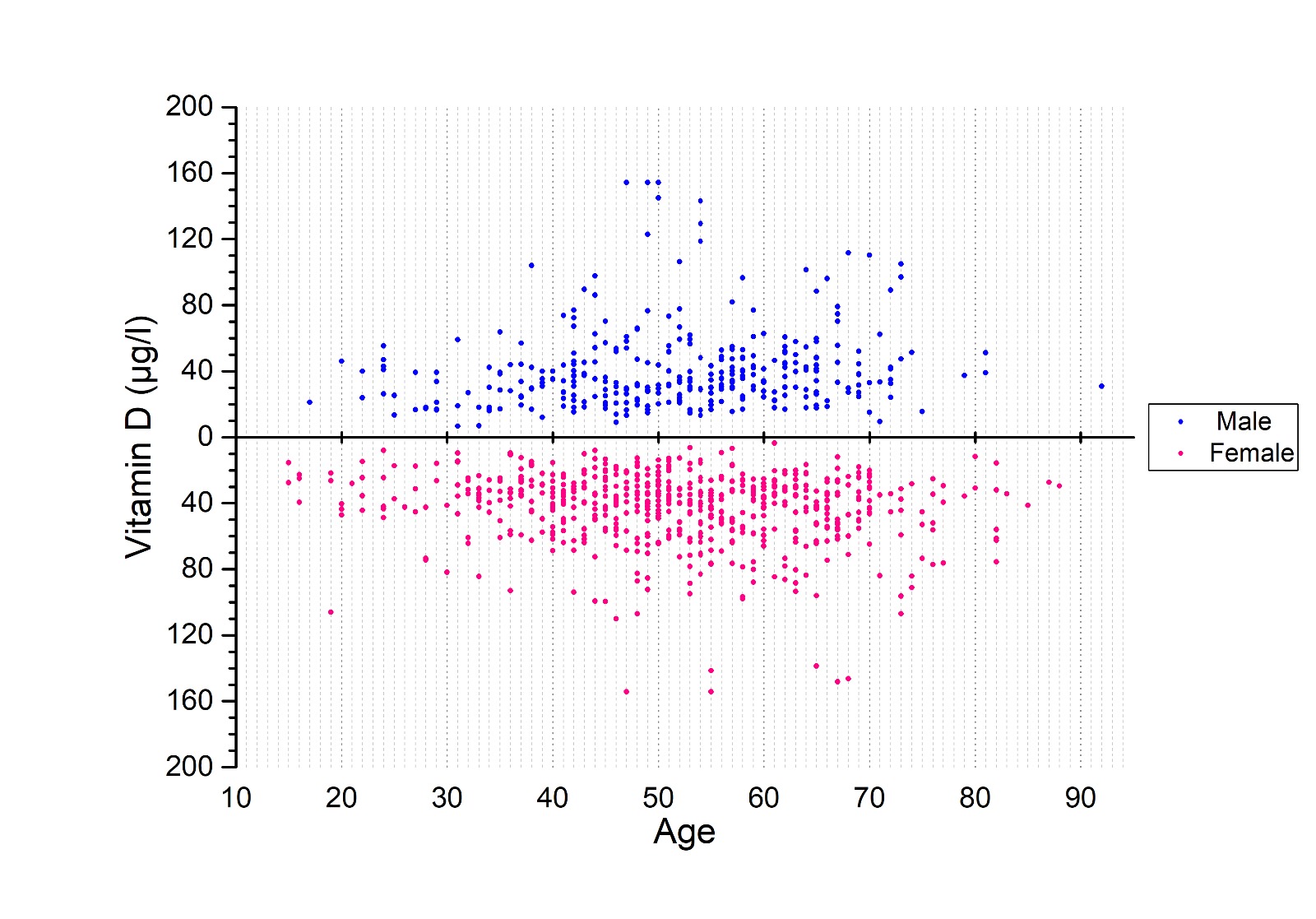
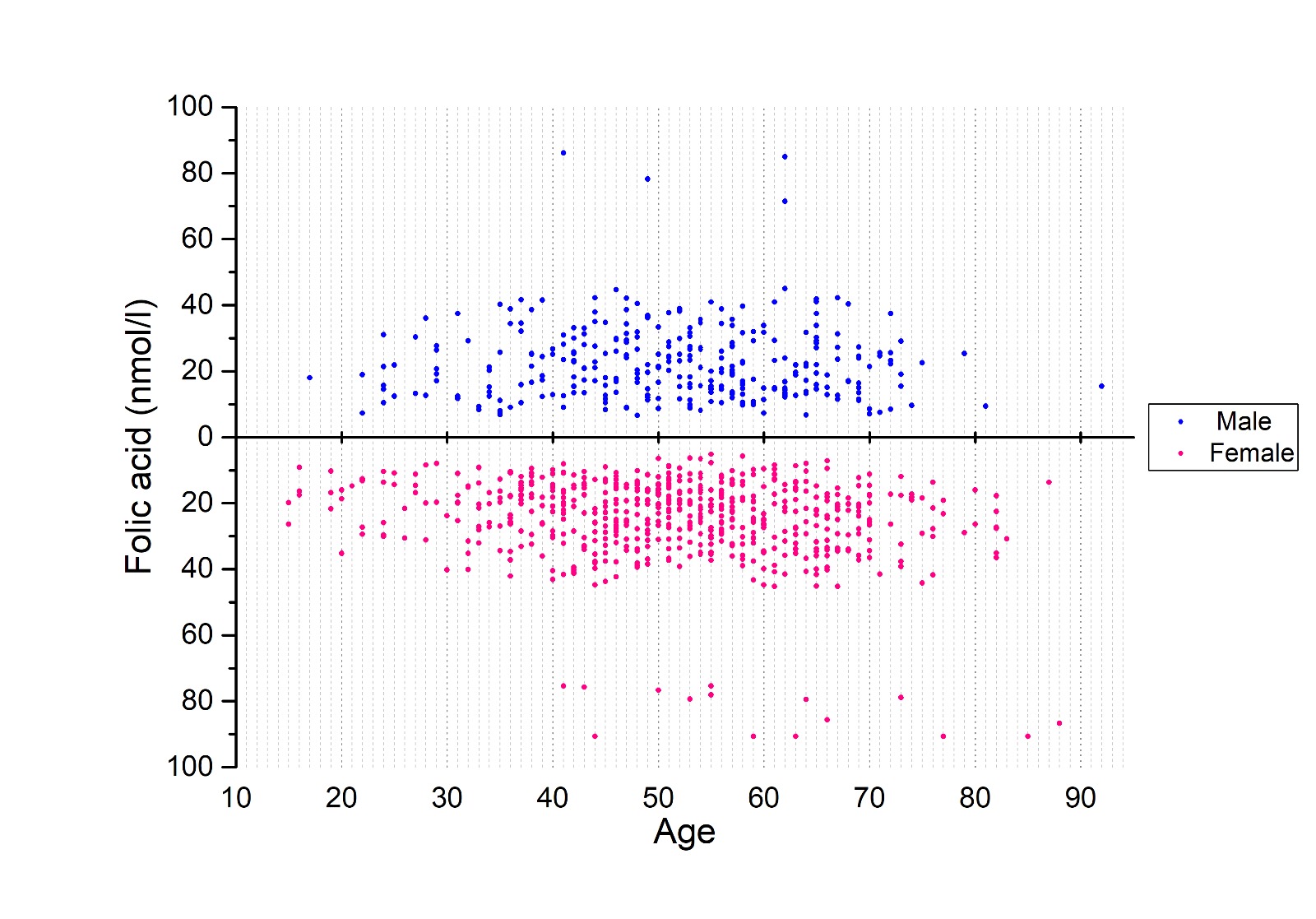
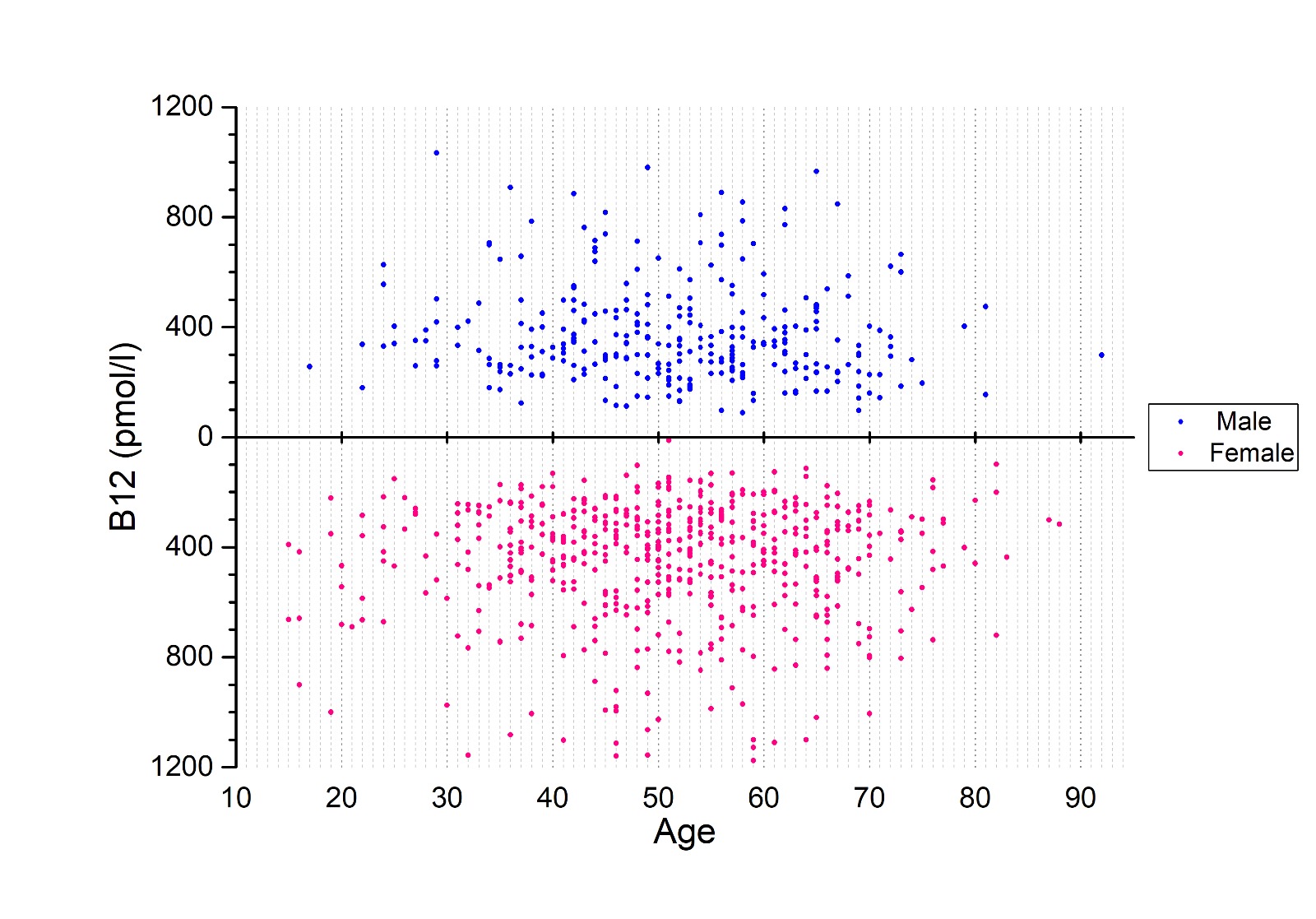
Issues with bone healing, particularly in relation to implants, have already been documented. It is well known that the immune system plays a significant role in bone health and disease. It also plays a crucial role in bone regeneration during the healing of bone wounds, including in the oral cavity. Chronic inflammation consistently leads to increased production of oxidants, and an imbalance between oxidants and antioxidants results in oxidative stress for the body. This stress causes damage at the cellular and molecular levels, ultimately leading to cell damage, DNA changes, and cell death, which, in turn, results in impaired wound healing. Following this example, we conducted an analysis of vitamin D levels in our patient population, with the findings displayed in the graph below. Additionally, his latest work was published in a new article this February, and those interested can follow it here.
The mouth, with its teeth, soft tissues, and bone, is truly unique, and there is no comparable situation elsewhere in the body. At this link, you can find a master’s thesis written in 2022 on this very topic, which thoroughly explains the entire concept of so-called Fatty Degenerative Osteonecrosis, or FDOJ.
Low concentrations of oxygen, vitamin D, antioxidants, and unregulated blood lipids increase the likelihood of a wound healing with fatty degenerative bone, creating a site of chronic release of the inflammatory mediator CCL5 and associated complications.
For an easier idea, perhaps an example of a patient with severe trigeminal neuralgia, M. Z., who was recently with us. This is what he said:
On 7/9/2021, the pain started in the upper right 5. Suddenly, he remembers exactly where he was, the tooth was with a pin, it started to hurt… He is in a lot of pain the whole time – 8 to 9 is the intensity, he cries from the pain. He had a tooth removed and it wasn’t any better, he had another six and seven removed and it wasn’t any better. Cold wind makes it worse. Before that, he used to walk 8 km every day, but since the pain, he doesn’t dare. In the upper right location, he feels swelling and numbness.
After carrying out the appropriate diagnostics, we removed the fatty degeneration and after two days he says that he feels only a little of the procedure. That terrible pain is gone. The measured tissue value of the chemokine CCL5 was increased by as much as 38 times the normal basal value, as it is called.
If we didn’t have the knowledge, we could call it incredible, but since we understand on a molecular level what is happening, it is completely clear why the neuralgia subsided. The gentleman is just one of many examples. You must be wondering if it can happen again? The answer is yes. The body, in the narrower sense of the bones and the immune system, must be provided with everything necessary for the wound to heal with healthy bone tissue, and only this guarantees long-term success. We have cases where the pain returns after about a month and a half. This means that the bone has healed again with fatty degeneration and CCL5 has reappeared.
CONCLUDING REMARKS
Fatty degeneration with osteonecrosis of the jaw bone secretes the inflammatory mediator CCL5, which primarily causes the development of trigeminal neuralgia. CCL5 has been shown to influence the onset of many modern systemic diseases, and modern science, of which we are a part, confirms that the jawbone is an important source of this aseptic inflammation.
SOURCES
- https://icosim.de/wp-content/uploads/2022/03/SGoedgedrag-MSc-Biomedical-Science-Literature-Thesis-A-Critical-look-at-Fatty-Degenerative-Osteonecrosis-of-the-jawbone-A-Controversy-in-Modern-Dentistry-.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10886049/pdf/bioengineering-11-00191.pdf
- https://www.nature.com/articles/s41598-018-19643-0
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8423937/
MAHA
Slovenska cesta 54, 1000 Ljubljana, Slovenija, Europe
Tel. +386 51 248 888
email: info@maha.clinic
Mon, Tue, Wed: 8:00 – 15:00
Thu: 12:30 – 20:00
Fri: 8:00 – 13:30
© Copyright 2024 – Maha / Privacy Policy /made by visualbraingravity