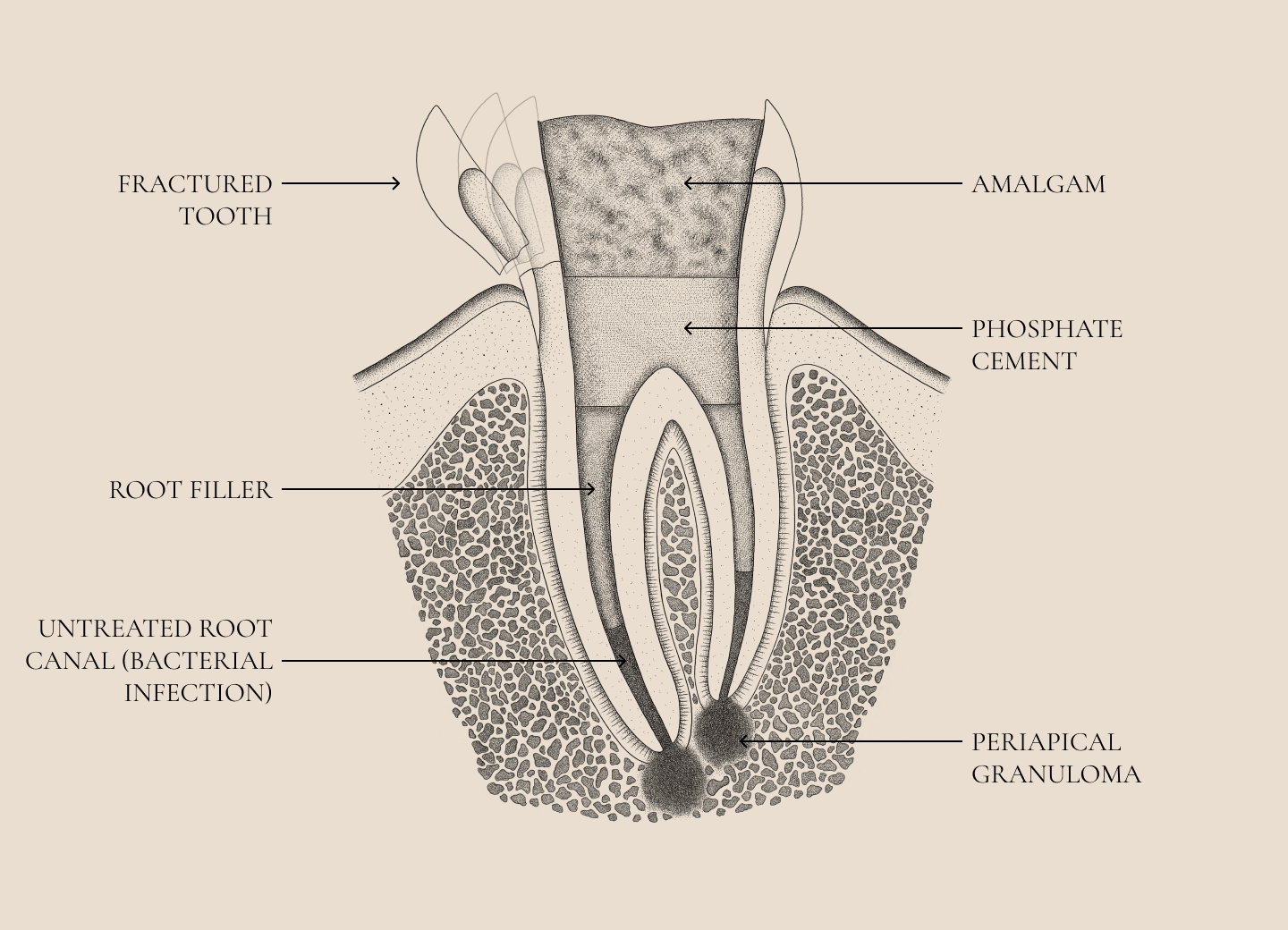
A lot of people ask themselves, should I just remove the dead tooth or should I save it? Endodontics, the branch of dentistry that focuses on dental nerve therapies or, more professionally, dental pulp and periapical conditions, in layman’s terms granulomas, is traditionally considered a localized procedure , designed to preserve natural teeth. However, recent evidence highlights the far-reaching consequences of root canal procedures on systemic health, suggesting that these procedures should not be considered in isolation, but rather as an integral part of your overall health care. At the end of the day, it is an infection similar to periodontal disease.
Systemic impact of endodontic infections
Endodontic infections, which also include “granuloma” or, more professionally, chronic apical periodontitis, are characterized by long-term inflammation and the presence of harmful bacteria that can also spread outside the mouth. These infections can trigger systemic inflammatory responses that contribute to the development or worsening of conditions such as cardiovascular disease, diabetes, adverse pregnancy outcomes, and others.
The spread of bacterial products such as lipopolysaccharides (LPS) into the bloodstream can cause a cascade of inflammatory processes that further link oral health to systemic diseases.
Linking infections within the tooth and periodontal tissues or more professionally the integration of endodontics and periodontology is an important modern field of dentistry and medicine. Considering the significant overlap of the effects of endodontic and periodontal diseases on systemic health, it makes sense to consider endodontics in the broader context of periodontology. Both areas deal with chronic oral infections that have systemic consequences. For example, periodontal disease, like untreated endodontic infections, is associated with chronic systemic inflammation, which is linked to diseases such as diabetes, heart disease, and even some cancers.
Treatment based on your systemic healthWhen planning endodontic therapies, the dentist must consider the systemic health of their patients. People can thus be divided into three groups:
Completely healthy individuals:
In this group, endodontic treatment can be performed using all modern methods for cleaning, disinfection and bioactive closure of the resulting space. We emphasize that this therapy cannot be performed without an operating microscope. Nevertheless, the potential systemic impact of any oral infection should not be neglected and the person should be informed accordingly. At the end of the day, it is a choice whether he decides to remove such a tooth or to treat it in the hands of the patient.
Early stages of the disease:
Patients showing early signs of systemic disease such as prediabetes, mild cardiovascular disease, incipient arthritis, etc., may be more susceptible to the systemic effects of endodontic infections. If you are dealing with diseases of this type and may already be taking medication, (Perhaps here is a link to the page where healthspan and diseasespan are explained), extremely consistent control of all infections and appropriate information are crucial, so that a person will be able to make decisions in accordance with modern findings of science.
Seriously ill patients:
In those with significant systemic conditions such as advanced diabetes, cancer, severe arthritis, fibromyalgia, etc. consideration of oral infections is crucial. The presence of endodontic infections can significantly worsen their systemic state of health, and in these cases, patients most often decide to remove such teeth.
The necessity of quality endodontic treatmentThe connection between endodontic and systemic health emphasizes the importance of accurate and high-quality diagnostics and taking action to care for the whole body and not just the local tooth. Suboptimal procedures leave residual infections that perpetuate systemic inflammation and contribute to the deterioration of your overall health.
CONCLUDING REMARKS
By recognizing the systemic effects of endodontic infections, dentists can make a significant contribution to improving your health outcomes, especially those with underlying and advanced systemic disease. An integrative approach requires a reconnection between medicine and dentistry to further validate these connections and refine treatment protocols.
SOURCES
- https://www.kcl.ac.uk/news/investigating-the-link-between-apical-periodontitis-and-cardiovascular-disease-risk
- Gomes, B. P. F. A., & Herrera, D. R. (2018). Etiologic Role of Root Canal Infection in Apical Periodontitis and Its Relationship with Systemic Diseases. Brazilian Oral Research, 32(suppl 1), e69. https://doi.org/10.1590/1807-3107bor-2018.vol32.0069
- Jiménez-Sánchez MC, Cabanillas-Balsera D, Areal-Quecuty V, Velasco-Ortega E, Martín-González J, Segura-Egea JJ. Cardiovascular diseases and apical periodontitis: association not always implies causality. Med Oral Patol Oral Cir Bucal. 2020 Sep 1;25(5):e652-e659. doi: 10.4317/medoral.23665. PMID: 32388515; PMCID: PMC7473437.
- Association between diabetes and the outcome of root canal treatment in adults: an umbrella review V. Nagendrababu, J. J. Segura-Egea, A. F Fouad, S. J. Pulikkotil, P. M. H. Dummer First published: 13 November 2019 https://doi.org/10.1111/iej.13253
- Caplan, D. J., Chasen, J. B., Krall, E. A., Cai, J., Kang, S., Garcia, R. I., & Offenbacher, S. (2006). Lesions of Endodontic Origin and Risk of Coronary Heart Disease. Journal of Dental Research, 85(11), 996–1000. https://doi.org/10.1177/154405910608501107
- Cotti, E., Dessì, C., Piras, A., Flore, G., & Deidda, M. (2011). Can a Chronic Dental Infection Be Considered a Cause of Cardiovascular Disease? A Review of the Literature. International Journal of Cardiology, 148(1), 4–10. https://doi.org/10.1016/j.ijcard.2010.08.004
- Siqueira JF Jr, Rôças IN. Present status and future directions: Microbiology of endodontic infections. Int Endod J. 2022 May;55 Suppl 3:512-530. doi: 10.1111/iej.13677. Epub 2022 Jan 13
- Hernández SR et al, Bacteriological conditions of the apical root canal system of teeth with and without post-treatment apical periodontitis. A correlative multi-analytical approach. J Endod. 2023 Nov 15:S0099-2399(23)00723-9. doi: 10.1016/j.joen.2023.11.005.
MAHA
Slovenska cesta 54, 1000 Ljubljana, Slovenija, Europe
Tel. +386 51 248 888
email: info@maha.clinic
Mon, Tue, Wed: 8:00 – 15:00
Thu: 12:30 – 20:00
Fri: 8:00 – 13:30
© Copyright 2024 – Maha / Privacy Policy /made by visualbraingravity