Dental diseases include the treatment of dental crowns and dental roots. We make sure your smile is healthy and beautiful. Proper oral health not only affects our appearance and self-image, it also affects our general health. “Dead” teeth have been haunting spirits for a long time and even today in the so-called developed society has no clear answers.
Several publications in scientific journals related to endodontics from 2023 state that endodontically treated, so-called “dead” teeth still contain bacteria in their hard tooth structure, dentin, meaning they are infected. Additionally, people are often confused as to why there are endodontic specialists, dentists who have dedicated their careers to treating tooth roots, and how it is that, in fact, every dentist performs the same therapies. “Why, what for?” is a common question in dental offices. Is it really worth saving every tooth at all costs, even if we feel it several times a year? The dentist sees nothing on the 3D X-ray, yet we still feel the tooth. What should we do? Is what we feel not right? I have cancer, arthritis, fibromyalgia, diabetes, neuralgia, and sometimes I feel discomfort in my jaw—what should be done in these cases?
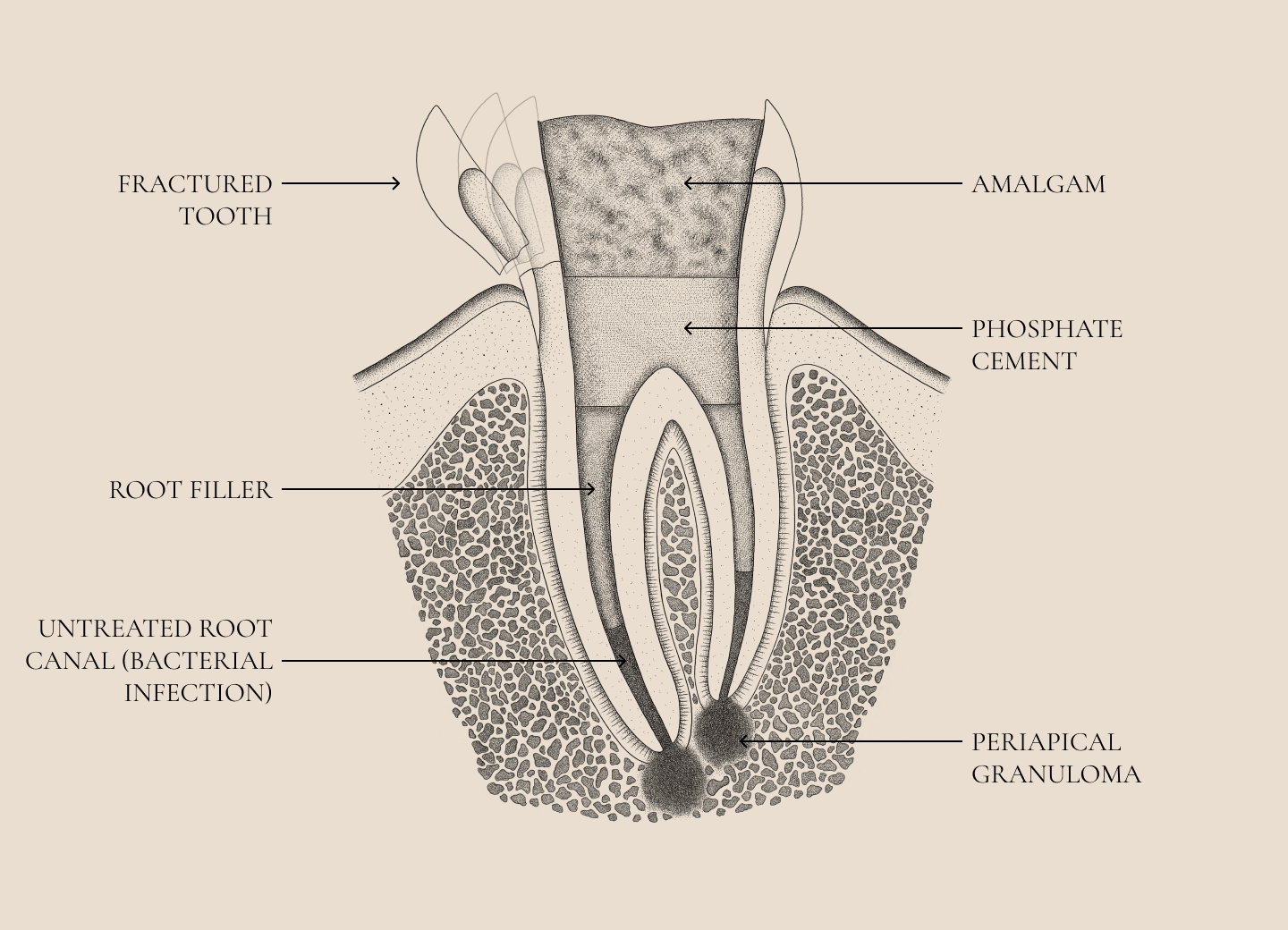
A tooth has its crown and root. Each tooth has a unique root shape and an even more unique shape of the canals inside, which are filled with blood vessels, nerves and Pischingers space. When the bacteria that cause tooth decay in the crown reach the root, where the so-called tooth nerve is, everything changes. Suddenly, we are no longer in the mouth, we ARE IN THE BODY. The hard tissue barrier is broken, and, if you will, the rules of the game change. Now the DENTIST becomes a DOCTOR. The bacteria have reached the dental pulp or the ‘nerve’ of the tooth and, through it, the bone at the end of the tooth root. Only in the bone can the body develop an immune response as a defense. Two problems arise.
- The canal through which the tooth ‘nerve’ runs is unfortunately not a straight tube inside the tooth, but rather a very branched canal structure, especially in the final parts of the roots called apices. In these branches, which cannot be reached during treatment, bacteria ‘nest.’
- The immune system, due to objective circumstances, simply cannot remove the bacteria within this complex canal structure.
Toppings
Each of us sooner or later faces tooth decay (caries).
Each of us sooner or later faces tooth decay (caries), and at that point, the decayed part of the tooth needs to be removed, and the missing tooth tissue replaced. As an alternative to traditional amalgam fillings, which are harmful to health and very unaesthetic, composite (white) fillings were introduced some time ago. With composite materials, we can restore your teeth with mechanically durable (strong) and highly aesthetic fillings, which primarily pose no risk to your health.
In most cases, we can restore teeth with smaller areas of decay so that your smile looks completely natural, even with fillings, as we have a wide range of color shades that match your teeth. The most modern materials are from the ORMOCER group and are also the most acceptable in integrative dentistry.
Tooth damage
Dental injuries are often an integral part of sports injuries, traffic accidents and other accidents.
Sooner or later, each of us faces tooth decay (caries) and then it is necessary to remove the tooth decay and replace the missing tooth tissue. As an alternative to traditional amalgam fillings, which are harmful to health and very unaesthetic, composite (white) fillings were created some time ago. With composite materials, we can restore your teeth with mechanically durable (strong) and highly aesthetic fillings, which first and foremost do not pose any risk to your health.
In most cases, teeth with smaller areas of tooth decay can be restored so that your smile looks completely natural despite fillings, as we have a wide range of color shades that match your teeth. The most modern materials are from the ORMOCER group and are also the most acceptable in integrative dentistry.
In cases of more extensive reconstructions of destroyed or cariously affected dental crowns, we decide on bioceramic restorations – partial ceramic coverings or “ceramic fillings”, which provide optimal care for teeth with a missing major part of the dental crown. Above all, bioceramic restorations are significantly more durable.
Granulom
"Granuloma" is usually a chronic inflammatory process of the body resulting from the action of bacteria from the root canal of the tooth in the bone around the end of the root.
Granuloma (Chronic periapical periodontitis):
Chronic periapical periodontitis, commonly known as granuloma, is a persistent inflammatory condition at the apex of the tooth root. It occurs as a defensive response to microbial infection in the root system and represents a significant proportion of infectious inflammatory conditions in dentistry. The treatment of chronic periapical periodontitis presents various challenges mainly due to the complex anatomy of the root canals.
Origin and course
It develops as a result of untreated or inadequately treated inflammation of the dental pulp or “nerve”, which often results from dental caries, injury or restorative interventions that threaten the pulp tissue. The dead pulp becomes a reservoir for microorganisms and their by-products, which spread through the opening at the end of the root into the tissues there and trigger an inflammatory response.
The body’s immune system responds by trying to limit the infection, leading to the formation of inflammatory tissue composed of connective cells, endothelial cells, and inflammatory cells. Over time, this inflamed tissue can persist or spread, causing the surrounding bone to disappear and appearing on X-rays as a dark area at the root apex.
Clinical presentation and diagnosis
People with granulomas may be asymptomatic or have mild symptoms such as discomfort when biting or slight tooth movement. Because of its gradual development, it is often discovered incidentally during routine X-ray examinations. It appears as a well-defined “black” area.
Treatment problems
The primary treatment method for chronic periapical periodontitis is non-surgical root canal therapy (RCT), which aims to eliminate the infection and promote healing. However, several factors contribute to the challenges for effective therapy:
- Complex root canal anatomy: Variations in root canal architecture, including accessory canals, apical deltas, and passageways, can harbor residual bacteria and dead tissue and impede complete disinfection.
- Microbial resistance: The presence of biofilms and resistant microbial species such as Enterococcus faecalis makes their eradication difficult. These microorganisms can survive in harsh conditions and are less susceptible to conventional agents.
Instrumentation and Irrigation Limitations: Mechanical treatment may not reach all areas of the root system, and irrigating solutions may have limited penetration and effectiveness, particularly in root-end regions. - Long-term inflammation: Even after appropriate therapy, residual inflammation may persist due to extra-root infections or reactions to extruded filling materials.
Patient factors: Systemic conditions such as diabetes or immunosuppression may impede healing and increase the risk of treatment failure.
Advanced treatment approaches
Various advanced processes and materials have been developed to solve many challenges:
- Improved irrigation techniques: Activation methods such as ultrasonic or laser-assisted irrigation improve the penetration and effectiveness of irrigants – FOTONA laser.
- Biocompatible filling materials: The use of materials such as mineral trioxide aggregate (MTA) allows for better sealing and periapical healing.
- Regenerative endodontics: Emerging therapies seek to regenerate pulp-like tissue and restore normal periapical tissues using stem cells and growth factors.
Concluding Remarks
Granuloma or Chronic periapical periodontitis represents a complex infection with significant treatment challenges due to anatomical complexity, microbial resistance, and patient-related factors. A thorough understanding of its pathogenesis and advances in endodontic techniques are essential to improve treatment outcomes. Clinicians must adopt a comprehensive approach on the basis of which we make appropriate decisions.
SOURCES
- Siqueira JF Jr, Rôças IN. Microbiology and treatment of acute apical abscesses. Clin Microbiol Rev. 2013;26(2):255-273.
- Nair PN. Pathogenesis of apical periodontitis and the causes of endodontic failures. Crit Rev Oral Biol Med. 2004;15(6):348-381.
- Lin LM, Huang GT, Rosenberg PA. Proliferation of epithelial cell rests, formation of periapical cysts, and regression of apical periodontitis. J Endod. 2007;33(8):908-916.
- White SC, Pharoah MJ. Oral Radiology: Principles and Interpretation. 7th ed. Mosby; 2014.
- Walton RE, Torabinejad M. Principles and Practice of Endodontics. 4th ed. Saunders; 2008.
- Lalonde ER, Luebke RG. The frequency and distribution of periapical cysts and granulomas. Oral Surg Oral Med Oral Pathol. 1968;25(6):861-868.
- Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984;58(5):589-599.
- Stuart CH, Schwartz SA, Beeson TJ, Owatz CB. Enterococcus faecalis: its role in root canal treatment failure and current concepts in retreatment. J Endod. 2006;32(2):93-98.
- Zehnder M. Root canal irrigants. J Endod. 2006;32(5):389-398.
- Siqueira JF Jr, Rôças IN. Extraradicular infection: a paradigm shift in endodontics. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(6):803-808.
- Fouad AF, Burleson J. The effect of diabetes mellitus on endodontic treatment outcome. J Am Dent Assoc. 2003;134(1):43-51.
- Simon JH, Enciso R, Malfaz JM, et al. Differential diagnosis of large periapical lesions using cone-beam computed tomography measurements and biopsy. J Endod. 2006;32(9):833-837.
- Garcez AS, Núñez SC, Azambuja N Jr, et al. Effects of photodynamic therapy on gram-positive and gram-negative bacterial biofilms. Photomed Laser Surg. 2013;31(2):77-84.
- Murray PE, Garcia-Godoy F, Hargreaves KM. Regenerative endodontics: a review of current status. J Endod. 2007;33(4):377-390.
MAHA
Slovenska cesta 54, 1000 Ljubljana, Slovenija, Europe
Tel. +386 51 248 888
email: info@maha.clinic
Mon, Tue, Wed: 8:00 – 15:00
Thu: 12:30 – 20:00
Fri: 8:00 – 13:30
© Copyright 2024 – Maha / Privacy Policy /made by visualbraingravity